Shoulder osteoarthritisis it chronic? a disease in which the articular cartilage tissue is destroyed and thinned, pathological changes occur in the soft tissues, and bone growths are formed in the joint area. It manifests itself with pain and crunching in the affected area. In the later stages, the range of motion decreases. The disease is chronic and progresses gradually. The diagnosis is made taking into account the clinical picture and radiological signs. Treatment is usually conservative: physiotherapy, anti-inflammatory drugs, chondroprotectors, physical therapy. When the joint is destroyed, arthroplasty is performed.
a disease in which the articular cartilage tissue is destroyed and thinned, pathological changes occur in the soft tissues, and bone growths are formed in the joint area. It manifests itself with pain and crunching in the affected area. In the later stages, the range of motion decreases. The disease is chronic and progresses gradually. The diagnosis is made taking into account the clinical picture and radiological signs. Treatment is usually conservative: physiotherapy, anti-inflammatory drugs, chondroprotectors, physical therapy. When the joint is destroyed, arthroplasty is performed.
General Information
Osteoarthritis of the shoulder joint is a chronic disease in which, as a result of degenerative-dystrophic processes, the cartilage and other tissues of the joint are gradually destroyed. Osteoarthritis usually affects people aged 45 years or older, but in some cases (after injury, inflammation), the disease can develop at a young age. Pathology occurs equally often in women and men, more often observed in athletes and people engaged in hard physical work.
The reasons
The starting point for changes in osteoarthritis of the shoulder joint can be both the normal aging process of the tissues and the damage or rupture of the cartilage structure due to mechanical influences and various pathological processes. Primary osteoarthritis is usually detected in the elderly, secondary (developed against the background of other diseases) can occur at any age. The main reasons are considered:
- Development defects. Pathology can be detected with underdevelopment of the head of the humerus or glenoid cavity, shoulder capomelia and other anomalies of the upper limb.
- Traumatic injury.Arthrosis of traumatic etiology occurs most often after intra-articular fractures. A possible cause of the disease can be a dislocation of the shoulder, especially the usual one. Less often, severe bruises serve as provoking injuries.
- Inflammatory processes.The disease can be diagnosed with long-term scapular periarthritis of the shoulder, previously non-specific purulent arthritis and joint-specific arthritis (with tuberculosis, syphilis and some other diseases).
Risk factors
Osteoarthritis is a polyetiological disease. There is a large group of factors that increase the likelihood of this pathology:
- Hereditary predisposition.Many patients have close relatives who also suffer from osteoarthritis, including those from other locations (gonarthrosis, coxarthrosis, arthrosis of the ankle joint).
- Joint overload.It can occur in volleyball players, tennis players, basketball players, throwers of sports equipment, as well as in people whose profession involves a constant high load on the hands (hammers, chargers).
- Other pathologies.Osteoarthritis is most often detected in patients suffering from autoimmune diseases (rheumatoid arthritis), some endocrine diseases and metabolic disorders, systemic insufficiency of the connective tissue and excessive joint mobility.
The likelihood of developing the disease greatly increases with age. Frequent hypothermia and unfavorable environmental conditions have a certain negative impact.
pathogenesis
The main reason for the development of arthrosis of the shoulder joint is a change in the structure of the articular cartilage. The cartilage loses its smoothness and elasticity, the sliding of the joint surfaces during movement becomes difficult. A microtrauma occurs, which leads to further deterioration of the condition of the cartilage tissue. Small pieces of cartilage detach from the surface, forming loose joint bodies, which also damage the inner surface of the joint.
Over time, the capsule and synovium thicken, areas of fibrous degeneration appear in them. Due to thinning and decreased elasticity, the cartilage ceases to provide the necessary shock absorption, therefore, the load on the underlying bone increases. The bone deforms and grows along the edges. The normal joint configuration is disrupted, there are movement restrictions.
Classification
In traumatology and orthopedics, a three-stage systematization is usually used, which reflects the severity of pathological changes and symptoms of arthrosis of the shoulder joint. This approach allows you to choose the optimal medical tactics, taking into account the severity of the process. The following phases are distinguished:
- The first- there are no gross changes in the cartilage tissue. The composition of the synovial fluid has changed, the nutrition of the cartilage is impaired. Cartilage does not tolerate stress, so joint pain (arthralgia) occurs from time to time.
- The second one- cartilage tissue begins to thin, its structure changes, the surface loses its smoothness, cysts and areas of calcification appear in the depths of the cartilage. The underlying bone is slightly deformed, bone growths appear along the edges of the joint platform. The pains become permanent.
- Third- marked thinning and rupture of the cartilage structure with extensive areas of destruction. The joint platform is deformed. Limitation of range of motion, weakness of the ligamentous apparatus and atrophy of the periarticular muscles revealed.
Symptoms
In the early stages, patients with osteoarthritis are concerned about discomfort or mild pain in the shoulder joint during exertion and certain body positions. Crunches may occur during movement. The joint has not changed externally, there is no edema. Then the intensity of pain increases, arthralgias become habitual, constant, appear not only during exercise, but also at rest, even at night. Distinctive features of the pain syndrome:
- Many patients note the dependence of the pain syndrome on weather conditions.
- Along with aching pain, over time, there is severe pain during physical exertion.
- Pain can occur only in the shoulder joint, radiate to the elbow joint, or spread throughout the arm. Possible back and neck pain on the affected side.
After a while, patients begin to notice noticeable morning stiffness in the joint. The range of motion decreases. After exercise or hypothermia, a slight swelling of the soft tissues is possible. As osteoarthritis progresses, movement is increasingly restricted, contractures develop, and limb function is severely impaired.
Diagnostics
The diagnosis is made by an orthopedic surgeon taking into account the clinical and radiological signs characteristic of arthrosis of the shoulder joint. If you suspect secondary osteoarthritis, consult a surgeon, an endocrinologist. At first, the joint is not changed, later it is sometimes deformed or enlarged. On palpation, the pain is determined. Movement restriction may be detected. To confirm osteoarthritis, the following is recommended:
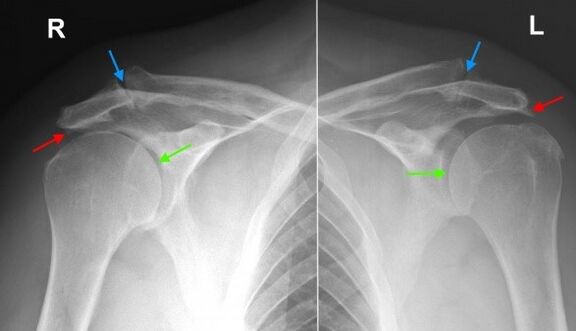
- X-ray of the shoulder joint.Dystrophic alterations and marginal bone growths (osteophytes) are found, in the following phases the joint space narrowing, deformation and changes in the underlying bone structure are determined. The joint gap can acquire a wedge-shaped shape, osteosclerotic changes and cystic formations are visible in the bone.
- Tomographic research.In doubtful cases, especially in the early stages of the disease, a CT scan of the shoulder joint is done to obtain additional data on the condition of the bone and cartilage. If it is necessary to evaluate the condition of the soft tissues, MRI is performed.
Differential diagnosis
Differential diagnosis of osteoarthritis is made with gouty, psoriatic, rheumatoid and reactive arthritis, as well as with pyrophosphate arthropathy. With arthritis, a blood test shows signs of inflammation; changes on radiographs are not very pronounced, osteophytes are absent, there are no signs of deformation of the articular surfaces.
In psoriatic arthritis, along with joint manifestations, rashes are often found. In rheumatoid arthritis, a positive rheumatoid factor is determined. With pyrophosphate arthropathy and gouty arthritis, biochemical blood analysis reveals corresponding changes (an increase in the level of uric acid salts, etc. ).
Shoulder osteoarthritis treatment
Patients are supervised by an orthopedic surgeon. It is necessary to limit the load on the arm, excluding sudden movements, lifting and prolonged carrying of weights. At the same time, it should be borne in mind that inaction also adversely affects the diseased joint. To maintain the muscles in a normal state, as well as to restore the shoulder joint, it is necessary to regularly carry out the physical therapy complex recommended by the doctor.
Conservative treatment
One of the most pressing tasks in osteoarthritis is the fight against pain. To eliminate pain and reduce inflammation, the following are prescribed:
- General acting drugs.NSAIDs are prescribed as tablets during an exacerbation. With uncontrolled use, they can irritate the stomach wall, have a negative effect on the state of the liver and metabolism in the cartilage tissue, so they are taken only as directed by a doctor.
- Local remedies.NSAIDs are commonly used in the form of gels and ointments. Self-administration is possible if symptoms occur or intensify. Less commonly, topical hormonal preparations are indicated, which should be applied according to the doctor's recommendations.
- Hormones for intra-articular administration.In case of severe pain syndrome, which cannot be eliminated by other methods, intra-articular administration of drugs (triamcinolone, hydrocortisone, etc. ) is performed. Blocks are carried out no more than 4 times a year.
To restore and strengthen cartilage in stages 1 and 2 of arthrosis, agents from the group of chondroprotectors are used: drugs containing hyaluronic acid, chondroitin sulfate and glucosamine. The treatment cycles are long (from 6 months to a year or more), the effect becomes evident after 3 or more months.
Physiotherapy treatment
With arthrosis of the shoulder joint, massage, physiotherapy exercises and physiotherapy techniques are actively used. During the remission period, patients are referred to spa treatments. To apply:
- mud therapy and paraffin;
- medicinal baths;
- infrared magnetotherapy and laser therapy;
- ultrasound.
Surgery
At stage 3 of the disease, with significant cartilage destruction, limited mobility and disability, joint replacement is performed. The referral for the operation is given taking into account the age of the patient, the level of his activity, the presence of severe chronic diseases. The use of modern ceramic, plastic and metal endoprostheses allows you to fully restore the function of the joint. The service life of the prostheses is 15 years or more.
Forecast
Osteoarthritis is a long-term, gradually progressive disease. It cannot be completely cured, however, it is possible to significantly slow down the development of pathological changes in the joint, preserve the ability to work and a high quality of life. To achieve maximum effect, the patient must be serious about his disease and his willingness to follow the doctor's recommendations, even during the period of remission.
Prophylaxis
Preventive measures include the reduction of domestic injuries, compliance with occupational safety, the elimination of excessive loads on the shoulder joint when performing professional tasks and playing sports. Pathologies that can cause the development of arthritic changes must be diagnosed and treated promptly.




































